Evolution of an Indication
How post-menopausal osteoporosis became a disease, and treatable
As the largest developed world population cohorts enter retirement, interest in ‘healthy aging’ surges. With more and more older adults, yet simultaneously fewer children, societies will need to find growth while providing for the needs of older adults.
Pharmaceuticals are a cost effective avenue to helping older adults age well. With drugs for age-related diseases like cardiovascular disease and osteoporosis help older adults stay stronger, longer.
While longevity enthusiasts dream of anti-aging cocktails, the story of post-menopausal osteoporosis offers an alternative path. Although post-menopausal osteoporosis is an age-related disorder, drugs that treat osteoporosis do not address underlying “mechanisms of aging,” but rather tackle the pathology directly. Bone frailty hasn’t been solved. But, development of pharmaceuticals has transformed post-menopausal osteoporosis from an unavoidable systemic burden into a manageable chronic condition. So, how did it happen?
Porous Bones
In the 1830s, French pathologist Jean Lobstein first described the porous, trabecular meshwork of bones from elderly skeletons. His observation helped explain what physicians long knew - fracture risk and bone fragility increase with age. Today we consider bone fragility a core component the frailty syndromes that many older adults experience. Many people still consider weak bones a normal, unavoidable consequence of aging. While age-related bone fragility has been known since antiquity, our understanding of bone fragility as a treatable condition emerged only in the 1940s.
From Phenomenon to Diagnosis
In 1940, at Massachusetts General Hospital, physician-scientist Fuller Albright first described the connection between menopause in women and bone loss. A physician-scientist, Fuller Albright developed interests in the medical mysteries of his patients at MGH. One such mystery was the pathological bone loss in largely middle aged women. This idiopathic osteoporosis was puzzling. In 1941, Albright, Smith, and Richardson authored "Postmenopausal Osteoporosis", a clinical description linking menopause, and the loss of endogenous estrogen production, as the probable driver of osteoporosis in middle-aged women.
Primarily interested in pathological fractures, such as compression fractures experienced during daily activities, the authors sought to link the bone fragility of the unexplained osteoporosis with an underlying pathological driver. By analyzing a cohort of young and middle aged women who experienced non-healing fractures, the authors concluded that the cases in their cohort lacked the deficiencies thought to drive bone loss in adults.
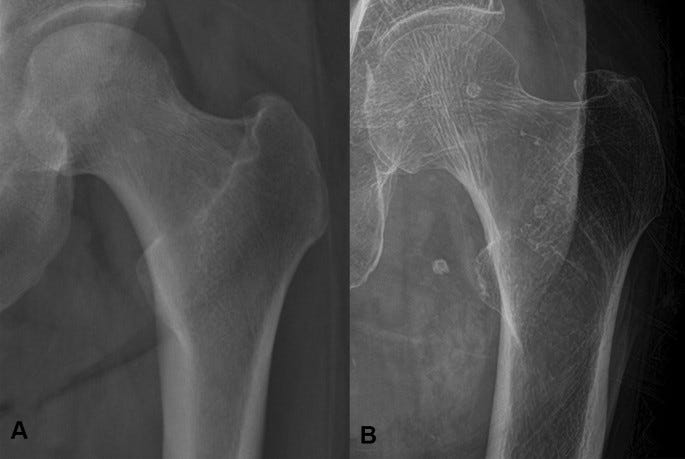
At the time, bone loss in adults was attributed to one of three factors: dietary insufficiency of calcium, vitamin D deficiency (as in rickets, osteomalacia), or lack of activity. Serum calcium and phosphorous levels were normal in the cohort. However, the authors’ cohort - active women and regular consumers of milk - had faint bone shadows on roentgenograms (X-ray images) and were susceptible to fractures during daily activities. Strikingly, these women with faint bone shadows were dramatically more likely to be experiencing menopause, early menopause, or artificial menopause via surgical oophorectomy. Rather ironically given the modern perception of post-menopausal osteoporosis as an age-related disorder, Albright, Smith, and Richardson specifically excluded cases of osteoporosis in patients over 65 in their identification because, in these patients, the condition could be confounded by age-related "senescence." Together, the evidence seemed to suggest that loss of ovarian function likely contributed to the increased bone fragility.
To pinpoint the etiology, Albright, Smith, and Richardson relied on new insights from skeletal biology. Recent work demonstrated that bone was not inert. Rather, it was constantly being disassembled and reformed by opposing sets of cells, osteoclasts and osteoblasts. Unlike rickets, osteoporosis is not a disease of calcium metabolism. Instead, osteoporosis appeared to be a disease of increased bone resorption and decreased bone deposition.
At the time, evidence that estrogen supplementation in humans could preserve and enhance bone mineral density was lacking. However, Albright, Smith, and Richardson were familiar with animal experiments in estrogen supplementation. In pigeons, investigators established a link between reproductive cycles and bone density. Estrogens can increase blood calcium levels in pigeons. Intriguingly, male pigeons almost uniformly have marrow filled long bones whereas female pigeons, at different points in the reproductive cycle, have either marrow filled long bones or near solid long bones. In fact, supplementing estrogen in male pigeons densified their bones. Similarly, in mice, estrogen supplementation can ossify long bones such that they nearly completely close marrow cavities. Citing evidence from estrogen supplementation in pigeons and mice, Albright, Smith, and Richardson proposed that estrogen directly promoted bone mineralization in humans and that its loss was the primary driver of osteoporosis in post-menopausal women. Later, Albright demonstrated that supplementation of certain sex steroid hormones - estrogen, progesterone, or testosterone - supplementation could preserve bone mineral content in post-menopausal and ‘senile’ osteoporosis, establishing post-menopausal osteoporosis as a treatable medical condition.
A Silent Epidemic Emerges
Yet, until the 1980s, few considered osteoporosis a major public health issue. What changed? In part, population aging. In the 1980s, the number of older adults grew as medical advances continued to curb major causes of premature mortality. Then, with more older adults, rates of geriatric health issues were increasing. From 1970 to 1984, hip fracture rates increased by 10%. This increase was concerning as, at the time, 20%-40% of women over 65 who fractured a hip would die within 6 months. In 1984, the NIH declared osteoporosis a “major public health problem” estimating that ≥1.3 million fragility fractures occurred in the US annually. Estimates of the annual cost to Medicare ranged from $3B-$5.2B as of 1986. At the time, these costs were about 4%-7% of Medicare’s annual budget ($74B USD). While already concerning, public health advocates feared the costs would grow as the early-Boomers turned 45 in 1990 and began to enter menopause en masse. Although the early-Boomers wouldn’t turn 65 until 2010, debilitating mid-life fractures in post-menopausal women could prematurely drain the workforce, increase disability-related care costs, and impair quality of life for women as they age.
However, some physicians argued that the age-related decline in bone density was merely a change in quantitative state, not a qualitative change from normal bone. Was the decrease in bone actually pathological? Physicians like Marshall R Urist, the co-discoverer of Bone Morphogenetic Proteins (BMPs), argued for a distinction between pathological and age-related osteoporosis. Urist argued that loss of bone mass in older adults is normal, time dependent, and coupled to reductions in muscle mass. In pathological osteoporosis, the rapid loss in bone mass “is characterized by spontaneous collapse of vertebral bodies [vertebrae] in the dorsal spine” (McLean and Urist. 1986. Bone. 239-240.). In patients with post-menopausal and age-related osteoporosis, external forces like accidental falls drove the fractures. So, was bone loss itself actually pathological?
Supplementation and Scare
While physicians argued the merits of estrogen replacement, pharmaceutical estrogens became widely available. Some physicians began supplementing estrogen in peri- and post-menopausal women to alleviate many symptoms of menopause - hot flashes, skin wrinkling, sexual dysfunction. Physicians and patients began to view menopause as a pathological sate of estrogen deficiency, not an unavoidable phase of life.
In 1966, Gynecologist Robert Wilson released “Feminine Forever,” a book extolling the virtues of estrogen supplementation during and after menopause. Reception was, at best, mixed. One scathing review in JAMA criticized the self-aggrandizing nature of the book (Wilson didn’t pioneer hormone replacement therapy as he claimed) and the reductive view of femininity (i.e. estrogen is what makes a woman). Later, it was revealed that the Wilson was paid by the manufacturer of Premarin1, a leading estrogen supplement of the era (Dominius, NYT). That year, prescriptions for Premarin doubled to 3.2M.
Simultaneously, the emergence of new technologies, such as bone morphometry, bone densitometry, and Dual Energy X-ray Absorptiometry (DXA), enhanced the quantification of bone mass and density. These new bone quantification techniques helped physicians more precisely quantify bone density and diagnose osteoporosis. Yet, diagnostic standards were highly variable and the primary treatment available to women was estrogen supplementation. While the NIH rang the alarm to alert the world to the serious public health issue of post-menopausal osteoporosis, concerns about estrogen replacement therapy surfaced.
Large observational studies in the 1980s identified a link between estrogen supplementation and breast cancer risk. The 1987 Cancer and Steroid Hormone (CASH) case-control study identified an 30% increased risk of developing breast cancer for women who had been supplementing estrogen after a bilateral oophorectomy. This cancer signal provided additional impetus for the FDA, and drug developers, to advance novel, non-hormonal osteoporosis therapies.
Drug Boom
At the time, patients lacked effective non-hormonal options to manage osteoporosis. But, that was about to change with the development of the bisphosphonate class.
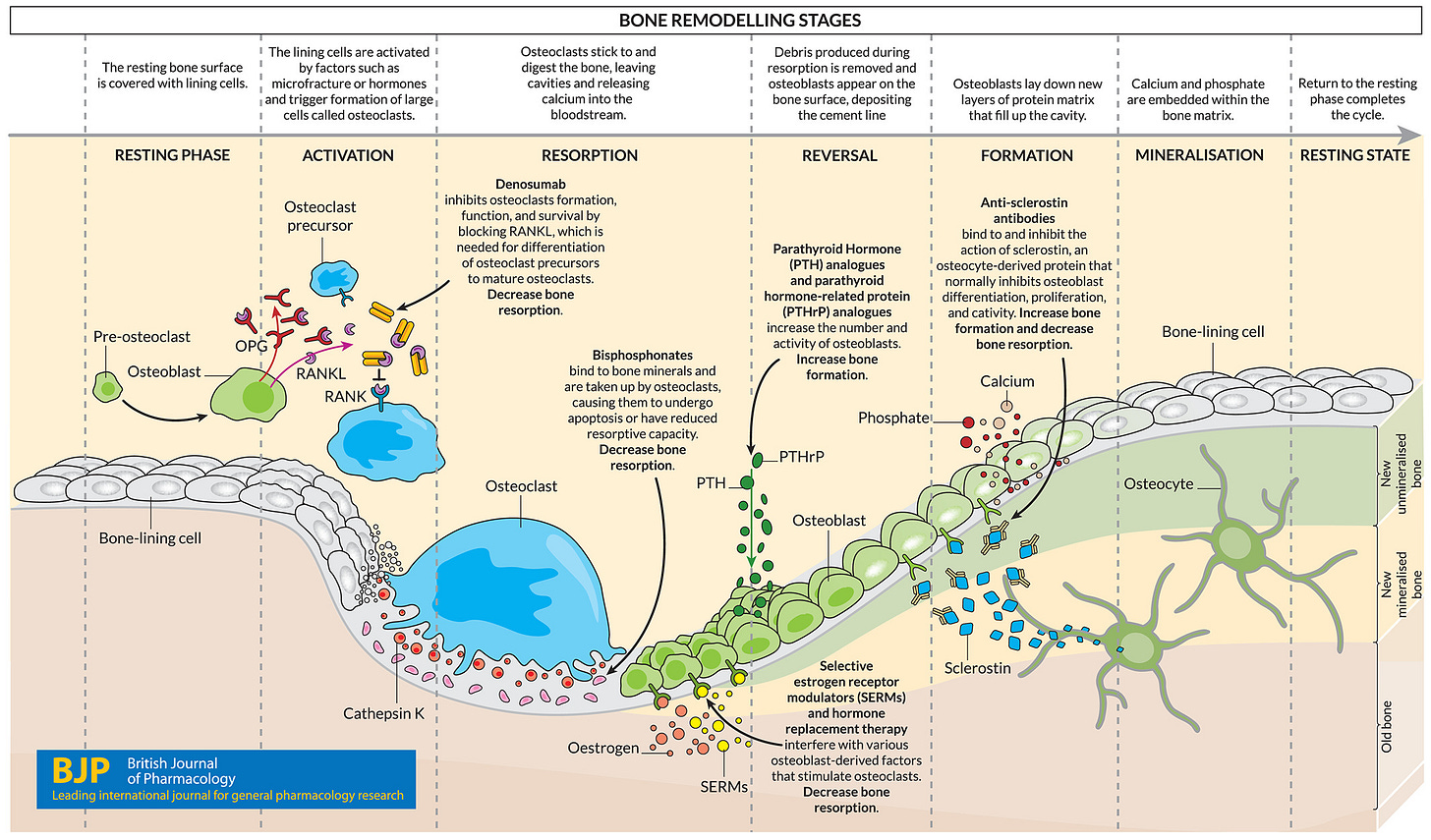
Initially synthesized as calcium chelating agents for use in industrial applications, bisphosphonates are organic analogs of inorganic pyrophosphates. In patients, bisphosphonates block bone resorption and new bone deposition. In 1969, Fleisch et al. demonstrated that organic bisphosphonates could prevent the formation and dissolution of hydroxyapatite, the major mineral constituent of bone. In that same paper, the authors also demonstrated that bisphosphonates could slow bone loss in an ovariectomized rat model of bone loss. The first bisphosphonate drug, etidronate, was approved in 1977 for use in treating Paget’s disease of bone, a bone formation disorder, and heterotopic ossification, a condition where soft tissue gradually forms bone. Although not approved to treat osteoporosis, the early generation bisphosphonates were used off label to manage the condition. However, in 1994, two decades after initial FDA approval, daily oral etidronate was first evaluated in a randomized controlled trial to assess its ability to treat osteoporosis. For patients with post-meonpausal osteoporosis, etidronate reduced fracture rates by more than 50% over two years.
In 1995, alendronate (Fosamax), a bisphosphonate 100-fold more potent than etidronate, won approval for the treatment of fracture risk in post-menopausal osteoporosis. Although effective, alondronate is not perfect. Up to 10% of patients experience esophageal inflammation while taking alondronate. To complement the bisphosphonate class, Selective Estrogen Receptor Modulators (SERMs), such as raloxifene which mimics estrogen in bone while blocking estrogen in the breast and uterus, were approved in the late 1990s.
Physicians and patients rapidly adopted bisphosphonates and SERMs. National office‑visit data show bisphosphonate or raloxifene use in osteoporosis visits rose from 14 % to 73 % (1994‑2003), while estrogen use fell sharply after 1995.
What helped accelerate the rapid uptake of SERMs and bisphosphonates? The causes are a bit overdetermined. In 1990, the first baby boomers began turning 45 and entering menopause, thus increasing the incidence of post-menopausal osteoporosis. Similarly, throughout the 1990s, there were sustained efforts by the public health establishment to promote the use of non-hormonal bone preserving therapies. Perhaps, most importantly, in 1994, the World Health Organization convened a meeting to define osteoporosis in terms of Bone Mineral Density (BMD) thresholds. The WHO aligned on a definition of osteoporosis as a BMD of 2.5 standard deviations below average *peak* bone mass, stratified by sex. So, a woman at age 70 could be ≤-1.0 SD below the mean for *age* and *sex*, but could also be clinically osteoporotic as their BMD could be below the 2 SD mean.
Normal: T ≥ -1.0 SD
Osteopenia (low bone mass): -1.0 > T > –2.5 SD
Osteoporosis: T ≤ -2.5 SD
Severe osteoporosis: T ≤ -2.5 SD plus ≥1 fragility fracture
In 2008, the University of Sheffield further refined the risk stratification of patients with the introduction of the FRAX algorithm. With country-specific models of fracture risk, FRAX helps physicians estimate the 10-year osteoporotic fracture risk of individual patients. Using BMD and individual patient history, FRAX can more precisely identify patients of concern (e.g. osteopenic T-score with history of glucocorticoid use).2
Prior to the WHO guidelines, multiple definitions of osteoporosis were in use. By unifying the indication definition with an accessible screening technology, DXA, the WHO opened the doors to widespread diagnosis. Introduction of tools like FRAX helped better identify high risk patients that would be otherwise missed. And, with bisphosphonates and SERMs, diagnosis became safely actionable.
In addition to helping identify patients, standardizing the diagnostic criteria also enabled drug developers to operate on a harmonized understanding of the indication. This certainty helped drug developers plan clinical evaluations of their therapies and project eligible populations. Further, the use of BMD T-scores (and then Z-scores, age-and-sex corrected BMD scales) Although these changes might seem trivial, pharmaceutical companies make decisions on the basis of risk-adjusted Net Present Value models of drug programs. Without an understanding of the eligible population or the anticipated drug effect, companies struggle to underwrite high-risk Phase 2 studies or a long Phase 3 outcomes study. When risk and reward are both highly uncertain, making decisions is uncertain.
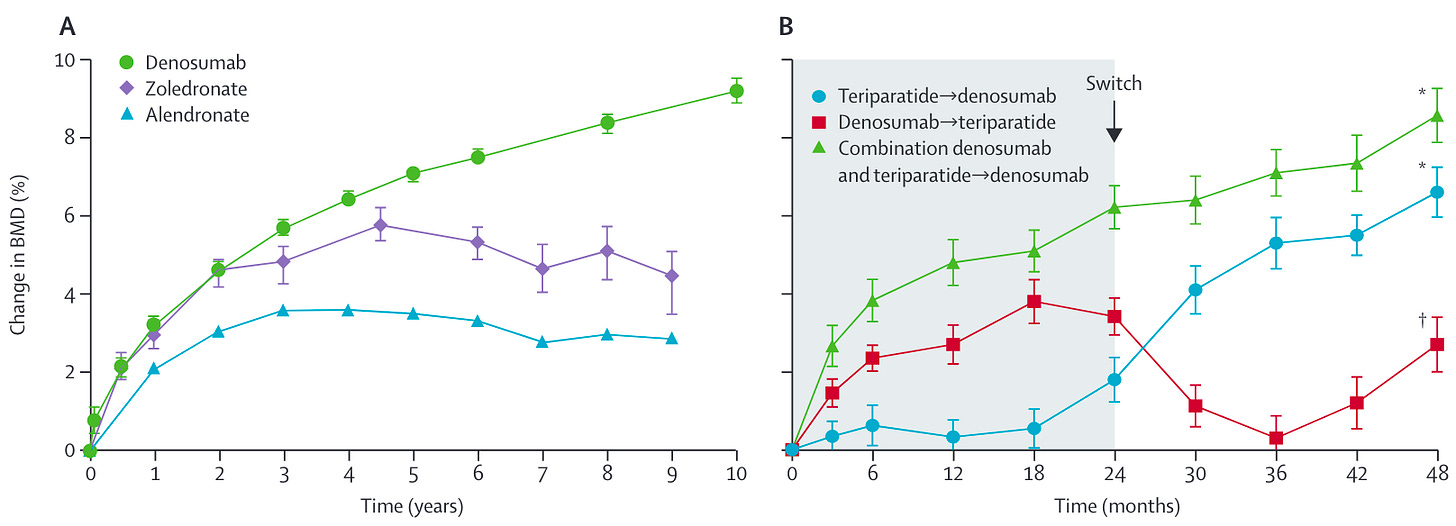
From the 1990s through the 2010s, pharmaceutical companies continued to invest in novel osteoporosis therapies. More active and longer acting bisphosphonates, like Ibandronate (Boniva) and Zoledronate (Reclast), continued to enter the market. However, bisphosphonates are not perfect. Interrupting bone-remodeling by osteoclast inhibition appears to increase the risk of atypical femoral fractures and osteonecrosis of the jaw3. To address these limitations, the early 2000s also saw the introduction of novel bone anabolic therapies for osteoporosis patients. In 2002, the FDA approved the first bone anabolic therapy, parathyroid hormone (teriparatide / Forteo, PTH 1-34). In 2010, Amgen brought the RANKL inhibitor denosumab (Prolia), a bi-annual biologic that blocks osteoclast resorptive action, to the osteoporosis market. RANKL inhibition rapidly increases bone mineral density by blocking bone resorption, but chronic RANKL inhibition increases the risk of Amgen extended their blockbuster osteoporosis franchise through the 2019 approval of romosozumab (Evenity), an anti-sclerostin antibody co-developed with UCB, which helps osteoblasts deposit more new bone. In 2017, Radius Health won approval of abaloparatide (Tymlos), recombinant parathyroid hormone related peptide, an alternative bone anabolic therapy.
Yet, osteoporosis is not a solved problem. While the clinical armamentarium of drugs to manage osteoporosis expanded rapidly since 1990, patients with osteoporosis still lack a convenient, long-term option to arrest the disease. Bisphosphonates remain first-line therapy. But, patient patient concerns about side-effects with chronic use limits their utility. While regular, transient exposure to teriparatide (PTH) can increase BMD, chronic use blunts the anabolic benefits of PTH and can lead to BMD decay. Abaloparatide was intended as a safer alternatitive to Lilly’s teriparatide. Sadly, approval of abaloparatide came with a Boxed Warning for increased risk of osteosarcoma (in animals) and hypercalcemia. Abaloparatide’s Boxed Warnings limited patient uptake of the drug. After years of lackluster sales, Patient Square Capital and Gurnet Point Capital took Radius Health private after the FDA removed the Boxed Warning for osteosarcoma. Romosozumab has a Boxed Warning for MI, stroke, and CV death.4 Together, these safety concerns limit widespread uptake of osteoporosis therapies. Today, perception of limited marketability has slowed much of the investment into much of the novel mechanisms.5
Instead, clinical innovation in osteoporosis tends to focus on sequencing existing therapies to maximize clinical benefit while reducing treatment burdens and improving patient experience. The figure below shows BMD changes from RCTs of post-menopausal osteoporosis patients comparing monotherapy interventions with cycling and combination therapies. While bisphosphonates and RANKL inhibitors remain first-line for osteoporosis, physicians lack consensus on optimal drug sequencing regimens.
Losing Ground
Between 1995 and 2010 - exactly the period in which DXA screening and bisphosphonate prescriptions soared - US hip-fracture incidence fell 42 % in adults ≥65 y/o. Other datasets that include vertebral and wrist fractures show a parallel 1-3 % annual decline. Economists estimate that the lives saved and nursing-home days averted generated social value far exceeding drug costs. The momentum stalled after 2012. Medicare claims reveal a slight rebound adding >11,000 excess hip fractures from 2013–2015 relative to prior projections. Three forces converged:
Therapy gaps. Only one quarter of women who meet National Osteoporosis Foundation treatment thresholds actually receive medication, and <23 % of fracture patients initiate therapy within a year.
Safety fears. Media reports on atypical femoral fractures and osteonecrosis of the jaw—rare but dramatic complications—coincided with a ≥50 % drop in oral bisphosphonate use between 2008 and 2012 after a decade of progress.
Screening cutbacks. Reimbursement cuts for office-based DXA in 2007 halved screening capacity, delaying detection of low bone mass just as the baby-boomer cohort entered retirement.
Unfortunately, like many degenerative diseases, prevention is complex. Patients don’t experience symptoms of osteoporosis until a fracture occurs. Osteoporosis is rarely actively painful. Unlike osteoarthritis where patients experience painful functional limitations daily activities, osteoporosis lacks the acute symptoms motivate diagnosis. Therefore, both providers and patients can lack urgency in addressing osteoporosis. Even with regular screening, many high-risk patients can go undiagnosed. Like age-related visual degeneration, symptoms may not appear until disease progression is advanced enough to limit therapeutic efficacy. Therefore, aggressive screening remains crucial to the prevent bone loss that drives fracture risk for older adults.
Lessons in avoiding the unavoidable
Over the course of the 20th century, post-menopausal osteoporosis evolved from a poorly understood phenomenon to a manageable chronic condition.6 Importantly, While post-menopausal osteoporosis is well characterized as driven by the decline in estrogen, the discovery and development of pharmaceutical approaches to prevent and treat age-related osteoporosis happened without a deep mechanistic understanding of the underlying drivers of bone loss with age. In both men and women, bones become more brittle with age.
Longevity enthusiasts dream of the FDA designating ‘aging’ as a disease. Although I think this impulse is directionally correct, it’s unclear what this would accomplish. However, the story of post-menopausal osteoporosis offers an alternative: go narrow. A narrow, functional definition of an age-related disorder effectively mobilized public health infrastructure, pharmaceutical firms, and investment capital. A well-defined patient population helped drug developers better assess both the treatment effect and the potential value to patients with the new drug. More certainty about the development risk, clinical need, and anticipated reward helped companies decide to allocate capital towards developing novel osteoporosis drugs. So, identify the need. Quantify it. Intervene in the highest need patients. Progressively expand to first-line prevention. Then, perhaps, if we follow this roadmap - define, quantify, intervene, expand - we can help older adults stay stronger, longer.
Premarin is a mixture of conjugated equine estrogens (CEEs) extracted from the urine of pregnant horses. Premarin is a contraction of “Pregnant Mares’ Urine.” Davis et al. 2005. JOE.reviews the various sources of estrogen for supplementation across history.
FRAX doesn’t capture all known risk factors for osteoporotic fractures. For example, the same group that developed FRAX identified type 2 diabetes as an independent risk factor - independent of BMD T-score and Z-score - for fractures in osteoporotic patients Giangregorio et al. 2012. JBMR.
Osteonecrosis of the jaw (ONJ) is rare but strongly linked to bisphosphonate use. The correlation had been observed in patients with multiple myeloma or metastatic breast cancer. Initially, ONJ was attributed to chemotherapy effects in cancer patients. However, this link was subsequently established in osteoporosis patients in 2008. Estimates place the risk of ONJ in osteoporosis patients in the range of 0.01-0.5% (after dental extraction). Following publication, the FDA revised the labels of bisophosphonates in 2011 to reflect the rare but serious side effect of ONJ (Zoledronate, Alendronate).
The causality of the signal has been contested, but human genetics - via Mendelian Randomization - suggests that lower blood sclerostin levels do predict increased BMD and increased CV risk in a dose-dependent fashion.
There are exceptions! Angitia is pursuing an dual anti-Wnt inhibitor (anti-DKK1 x anti-Sclerostin bi-specific antibody) based on prior work from Amgen. Angitia raised a $120M series C in December of 2024.
Historian Gerald Grob (1931-2015), published perhaps the most comprehensive article and book detailing the history of osteoporosis. After building a career writing about treatment of mental illness across time, Grob developed an interested in osteoporosis towards the end of his career. To my understanding, his work is the most comprehensive history of osteoporosis that directly tracks the transition from age-related phenomenon to treatable pathology. Grob is skeptical of the utility of broad intervention for primary prevention. But, his history is comprehensive nonetheless.
